Two Lives Saved

A MULTIDISCIPLINARY TEAM UNITES TO NAVIGATE
ONE OF THE MOST COMPLEX CASES IMAGINABLE
It took a dedicated team of over 100 doctors, nurses, and other professionals from UK HealthCare to save Sarah Custer and her baby.
The critical factor was a new drug resulting from a clinical trial that ultimately put Sarah’s cancer into remission. It’s the type of treatment only available at specialized institutions like the UK Markey Cancer Center, Kentucky’s Comprehensive Cancer Center designated by the National Cancer Institute.
Stage 4 Lung Cancer
Sarah and her husband, Dave, were living a quaint life with their growing family in Columbia, a small town in south-central Kentucky, when she received a daunting cancer diagnosis.
In early August 2021, the young couple contracted COVID-19 while Sarah was pregnant with their third child, Isabel. After a few weeks, Dave’s cough went away, but Sarah’s lasted into September. By month’s end, she was coughing blood and vomiting.
Scans showed a large soft-tissue mass blocking both airways in her lungs and causing respiratory failure. She was struggling to breathe and needed 10 liters of oxygen. Dr. Ashish Maskey, Markey’s director of bronchoscopy and interventional pulmonary, suspected Sarah had stage 4 lung cancer.
Maskey’s sense of urgency in developing a plan prioritizing both Sarah’s and Isabel’s needs gave the Custers hope. Before deciding how to proceed, he needed to biopsy the mass in Sarah’s lungs and place a stent to improve her breathing. That called for a bronchoscopy, a typically routine surgery. However, this one would be difficult given the circumstances, as fluctuations in oxygen level during the procedure could have harmed both Sarah and baby Isabel. So, Sarah had to be placed on extracorporeal membrane oxygenation, or ECMO — a heart-lung machine representing the most advanced form of life support.

Cardiologists Dr. Rajasekhar Malyala and Dr. Jonathan Steyn oversaw the ECMO as Maskey performed the bronchoscopy. Dr. Sumit Dang and Dr. John O’Brien – both specialists in highrisk pregnancies – monitored Isabel’s vitals throughout. Sarah was off ECMO a few days later, breathing easier and considering options to treat her cancer while prioritizing her unborn daughter’s safety.
‘We Had to Save Both’
But after 12 days at home, Sarah was rushed back to Lexington. The lung mass had grown, dislodging the stent and sending her into respiratory failure. Her life and Isabel’s were in jeopardy.
“It literally felt like I was trying to suck my life’s air through a straw that somebody was pinching,” Sarah said.
The cancer had spread rapidly to her brain, spine and hips. She also had fractured vertebrae in her back that required surgery.
“When I talked to Sarah, she said, ‘Save my baby,’” Maskey said. “But when she went on the ventilator, her husband said, ‘Save my wife.’ But it’s not a choice. We had to save both.”
O’Brien delivered Isabel by C-section at 32 weeks before Maskey placed a new stent. Throughout her multiple surgeries, Sarah was intubated – with a tube inserted into her throat to open her airway. Doctors waited about a week to take the tube out. Soon after she awoke, Sarah held Isabel for the first time, not knowing if she’d get the chance again.
Targeted Cancer Drug
Around that time, the results from Sarah’s initial biopsy came in. Dr. Ralph Zinner, director of Markey’s thoracic oncology program, explained that Sarah had “an extraordinarily high concentration” of a rare mutation of anaplastic lymphoma kinase (ALK), a gene that helps in the development of the gut and nervous system in embryos. About 4 percent of lung cancers test positive for ALK, and of that 4 percent almost all are adenocarcinoma nonsmall cell lung cancer, as Sarah’s was.
After some setbacks, Sarah started a course of treatment that included alectinib. This targeted cancer drug blocks the activity of ALK. Alectinib, sold under the brand name Alecensa, was first approved for use by the U.S. Food and Drug Administration in 2015. In late 2017, it gained first-line treatment approval for ALK-positive metastatic non-small cell lung cancer. In April 2024, it gained FDA approval as a first adjuvant treatment.
Sarah’s cancer receded as quickly as it had spread, and she was able to hold Isabel again — this time knowing it wouldn’t be the last.
Cancer-free
A year later, Sarah was officially declared cancer-free. Alectinib’s effectiveness in treating cancers like Sarah’s, as observed through ongoing clinical research at Markey and other leading hospitals, has been eye-opening.
“Her tumors not only shrank, but shrank incredibly rapidly,” Zinner said. “It just suggests profound efficacy, and we are seeing patients on this drug having no evidence of cancer coming back years and years later.”
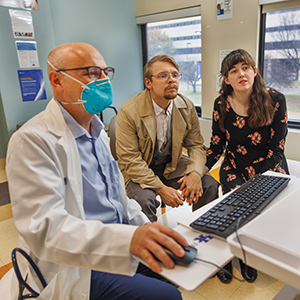
‘Never a One-doctor Show’
Sarah and Isabel’s journey required the kind of specialized team of medical experts you only find at one of the nation’s best hospitals.
“...All that training that we did is meant for these isolated, rare cases where we really put our skill to work. It is the biggest gratification for us to be able to help somebody and have them do well,” Maskey said.




