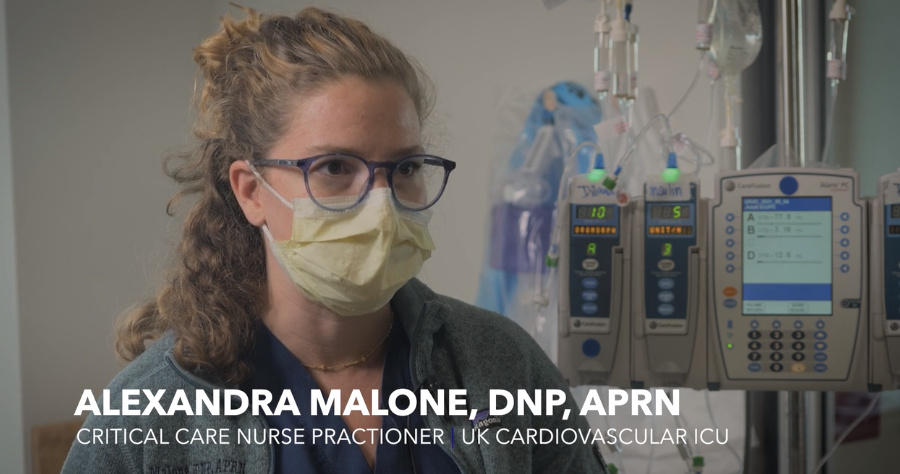
Voices from the Front Lines: Alexandra Malone
We recently joined hospital staff for a few days to document the reality of treating COVID-19 patients in UK HealthCare clinical settings.
This edited interview is part of our ongoing series, “UK HealthCare: Voices from the Front Lines,” highlighting stories and perspectives from our frontline staff who care for the sickest COVID-19 patients since March 2020.
Alexandra Malone is a nurse practitioner for the Critical Care Team.
Tell me a little bit about your job prior to COVID
I started as a nurse practitioner fellow in our CCM department in October of 2019, and it was supposed to go for a full year. Then COVID happened in March of 2020.
It was just (we) needed a lot of hands, so I was out of my fellowship a little bit earlier than expected. Prior to that, I was in the neuro and neurosurgical ICU a lot-- some surgical ICU, too.
In the beginning, we saw a lot of our elective cases go down. So, when I was on our surgical service, we would very frequently have maybe four patients on our list.
We didn't know how heavy we would be hit, essentially, how many cases we would see. So, we were just kind of always in a state of anxiety of, ‘when will we get pulled to work in the COVID ICU? When will we be pulled to go somewhere else or do something else?’
Now we're in our second surge, and things are just kind of changing again. We're having to be a little bit more flexible. We're getting a lot more patients who are sicker and younger, and that's just kind of affected how we've had to go about things.
We had to create a whole new team that deals with ECMO patients specifically. We're seeing more ECMOs than we have ever seen.
Can you tell me a little bit about what you all do for the COVID patients who come to this floor?
If they come to this floor, it's for ECMO specifically. So, we have to cannulate them to put them on a machine that takes all of their blood out of their body, circulates it through a machine to get oxygen, and then put it back in their body.
So, we're putting big cannulas in their neck to recirculate their blood and make sure it's getting the oxygen it needs, because their lungs can't do it for them. The COVID patients we're seeing are very, very sick on this floor specifically. And they're sick upstairs, too.
This particular surge seems to be really bad. Can you tell me what it’s been like for you?
Stressful. So, I'm originally from Arkansas. And I have been hearing for the last month about how the hospital I used to work at that all my friends are at has been at capacity for a month now. And a lot of young deaths — they are seeing a lot of 20- and 30-year-olds dying. I had somebody I know from high school who died this week.
We're seeing a lot of 20-year-olds, 30-year-olds, 40-year-olds on ECMO. And they're just not recovering as fast as we would like them to.
So, it's just been a little bit more stressful than the first go, because you're seeing younger people who are sicker than you would ever expect them to be and just all of the nursing staff and the rest of the hospital staff (is) being stretched thin because the volume has just increased drastically.
What's the most important thing that you want people out there to know about what's happening inside the hospital?
Just the toll that it's taking on all of the hospital resources, because we want to care for everybody. And we want to be able to have the ability to care for everybody. But with numbers just increasing, it's made it very hard to be able to do so.
We don't have machines for everybody, for every 20- 30-year-old that gets sick. We don't have the capability to place them all on ECMO. And it's just so important that everybody gets vaccinated so we don't have to use these machines for them, because there aren't enough.
What keeps you motivated to keep coming back here every day and treat these patients?
Just the desire to see something good happen for one of them. There's not been too many good outcomes, but you get to know the families. And you just really hope for the best. So, you just want to see improvements every day.
Do you have any sort of moment that has stuck with you, good or bad, while dealing with COVID?
I hate to be negative. There just hasn't been a lot of good, I feel like, because there are still so many people who are so adamant about not getting vaccinated. But they're not seeing how it's affecting everybody here and how we are all fighting for people to stay alive.
And it's hard to keep doing that when there are so many people who don't believe the vaccines work. But all the hospitals can see that most of our patients are unvaccinated. And we know that they work.
They're going to keep you from being hospitalized for long periods of time or as sick as you could be. And I feel like it's worse this time around, now that we have an option to help people. And people are just refusing to get it.
Everybody is so much sicker this time around. It's unreal how many people you see that are getting sick and getting very, very sick. And so, just it's very important that you just get vaccinated, essentially. That's the easiest thing that anybody could do to help anybody else around them is to just get vaccinated and wear a mask.




